Micro-TESE
Make an Appointment
Understanding Micro-TESE
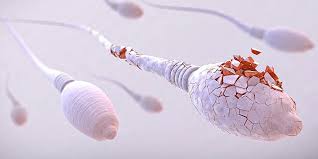
Micro-TESE is a highly specialized surgical procedure designed to retrieve sperm from the testicles of men with non-obstructive azoospermia. Unlike other sperm retrieval methods, such as conventional testicular sperm extraction (TESE), Micro-TESE utilizes an operating microscope, enabling surgeons to identify areas of the testicles with a higher likelihood of containing sperm.
During the procedure, a small incision is made in the scrotum, and the testicular tissue is carefully dissected using high-powered magnification. By visualizing the seminiferous tubules, which house the sperm-producing cells, the surgeon can identify areas with signs of active sperm production. This targeted approach increases the chances of retrieving viable sperm for use in assisted reproductive technologies.
Benefits of Micro-TESE
Improved Sperm Retrieval Rates: Micro-TESE has shown superior sperm retrieval rates compared to other techniques for non-obstructive azoospermia. By utilizing high-powered magnification, surgeons can identify testicular areas with active sperm production, increasing the likelihood of finding viable sperm. This precise and targeted approach minimizes unnecessary tissue sampling and maximizes the chances of successful sperm retrieval.
Minimally Invasive and Tissue-Sparing: Micro-TESE is a minimally invasive procedure that aims to spare healthy testicular tissue. By using an operating microscope, the surgeon can selectively dissect the testicular tissue, reducing the risk of unnecessary damage to healthy areas. This approach is particularly important for individuals with limited sperm production, as it optimizes the chances of finding viable sperm while preserving as much healthy tissue as possible for potential future procedures.
Potential for Future Treatments: Micro-TESE not only offers immediate benefits but also holds potential for future treatments. The retrieved sperm can be cryopreserved for future use, allowing individuals to undergo multiple cycles of assisted reproductive technologies without the need for additional surgical procedures. Additionally, the preserved tissue can be utilized for research purposes or emerging treatments, such as testicular tissue grafting or stem cell-based therapies.
Personalized Approach: Each individual’s testicular tissue is unique, and the sperm production pattern can vary. Micro-TESE allows for a personalized approach, as surgeons can assess the testicular tissue in real-time and tailor the procedure to the specific needs of the patient. This individualized approach improves the chances of successful sperm retrieval and increases the overall effectiveness of subsequent assisted reproductive technologies.
Conclusion
Micro-TESE represents a remarkable advancement in male infertility treatment, providing new possibilities for individuals with non-obstructive azoospermia. Through the use of an operating microscope, this specialized procedure offers higher sperm retrieval rates while minimizing invasiveness and preserving healthy testicular tissue. With its potential for future treatments and personalized approach, Micro-TESE holds great promise for individuals and couples struggling with male factor infertility. As technology and expertise continue to evolve, Micro-TESE will likely become an increasingly integral part of assisted reproductive technologies, offering renewed hope and the possibility of biological parenthood.
